Urinary Tract Infections in Karbala Population: Epidemiology, Causes and Treatment Options
DOI:
https://doi.org/10.59675/M313Keywords:
Urinary tract infections, Microorganisms, and Antibiotics.Abstract
Aim of study: To identify the etiological agent of urinary tract infections and test the sensitivity of microorganisms that caused UTIs to antibiotics. The study also aims to find the appropriate treatment that bacteria cannot resist or to find an alternative to it in treating urinary tract infections.
Methods: This was conducted at the microbiology department of the Al-Imam Al-Hussein Medical City in Karbala. Urine samples were collected from patients of different ages and sex. Bacterial culture and antibiotic susceptibility were performed in the laboratory. Many symptoms diagnose urinary tract infections (UTIs) by examining urine samples and bacterial growth on Petri dishes. There is a significant risk because of the increase in protract infections and the growing antibiotic resistance leading to the increase of the economic burden of these illnesses.
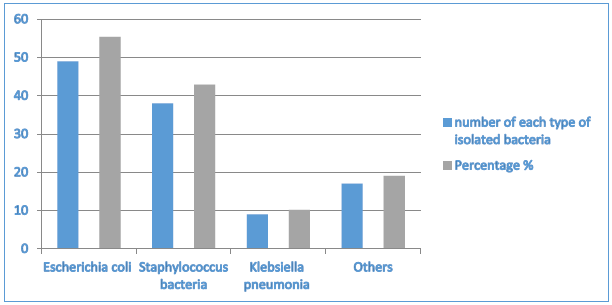
Results: UTI cultured samples included 30 males (26.5%) and 83 females (73.5%), with patient ages ranging from 18 to 90. Among 113 individuals with uropathogens, Escherichia coli in 49 patients (55.37%), followed by Staphylococcus bacteria detected in 38 patients (42.94%). Klebsiella pneumonia was detected in only 9 patients (10.17%), while other types of bacteria were detected in 17 (19%). Various antimicrobial agents were employed on the isolated bacteria; the highest sensitivity was observed for meropenem (79.5%), while the lowest sensitivity was noted for ampicillin (21.2%). Conclusion: Early diagnosis and treatment of UTI is very important to minimise medical complications and decrease financial outcomes; this is achieved by isolating the causative pathogens and testing for suitable antimicrobial drugs.
References
O’Brien VP, Dorsey DA, Hannan TJ, Hultgren SJ. Host restriction of Escherichia coli recurrent urinary tract infection occurs in a bacterial strain-specific manner. PLoS Pathog. 2018;14(12):e1007457.
Tamadonfar KO, Omattage NS, Spaulding CN, Hultgren SJ. Reaching the end of the line: urinary tract infections. Microbiol Spectr. 2019;7(3):10-1128.
Behzadi P, Urbán E, Matuz M, Benkő R, Gajdács M. The role of gram-negative bacteria in urinary tract infections: current concepts and therapeutic options. Adv Microbiol Infect Dis Public Health. 2021;15:35-69.
Klein RD, Hultgren SJ. Urinary tract infections: microbial pathogenesis, host-pathogen interactions, and new treatment strategies. Nat Rev Microbiol. 2020;18(4):211-226.
Klein RD, Hultgren SJ. Urinary tract infections: microbial pathogenesis, host-pathogen interactions and new treatment strategies. Nat Rev Microbiol. 2020;18(4):211-226.
Wagenlehner FM, Bjerklund Johansen TE, Cai T, Koves B, Kranz J, Pilatz A, et al. Epidemiology, definition and treatment of complicated urinary tract infections. Nat Rev Urol. 2020;17(10):586-600.
Hooton TM. Uncomplicated urinary tract infection. N Engl J Med. 2012;366(11):1028-1037.
Hummers-Pradier E, Kochen MM. Urinary tract infections in adult general practice patients. Br J Gen Pract. 2002;52(482):752-761.
Bonkat G, Pickard R, Bartoletti R, Bruyère F, Geerlings S, Wagenlehner F, et al. Urological infections. Arnhem: European Association of Urology; 2018.
Bono MJ, Leslie SW, Reygaert WC. Urinary tract infection.
Medina M, Castillo-Pino E. An introduction to the epidemiology and burden of urinary tract infections. Ther Adv Urol. 2019;11:1756287219832172.
Klein RD, Hultgren SJ. Urinary tract infections: microbial pathogenesis, host-pathogen interactions, and new treatment strategies. Nat Rev Microbiol. 2020;18(4):211-226.
Zhou Y, Zhou Z, Zheng L, Gong Z, Li Y, Jin Y, et al. Urinary tract infections caused by uropathogenic Escherichia coli: mechanisms of infection and treatment options. Int J Mol Sci. 2023;24(13):10537.
Flores-Mireles AL, Walker JN, Caparon M, Hultgren SJ. Urinary tract infections: epidemiology, mechanisms of infection and treatment options. Nat Rev Microbiol. 2015;13(5):269-284.
Pardeshi P. Prevalence of urinary tract infections and current scenario of antibiotic susceptibility pattern of bacteria causing UTI. Indian J Microbiol Res. 2018;5(3):334-338.
Pardeshi P. Prevalence of urinary tract infections and current scenario of antibiotic susceptibility pattern of bacteria causing UTI. Indian J Microbiol Res. 2018;5(3):334-338.
Abejew AA, Denboba AA, Mekonnen AG. Prevalence and antibiotic resistance pattern of urinary tract bacterial infections in Dessie area, North-East Ethiopia. BMC Res Notes. 2014;7:1-7.
Sood S, Gupta R. Antibiotic resistance pattern of community acquired uropathogens at a tertiary care hospital in Jaipur, Rajasthan. Indian J Community Med. 2012;37(1):39-44.
Agbagwa OE, Ifeanacho EJ. The prevalence of UTI pathogens in urine specimen obtained from a hospital in Rivers State Nigeria. J Microbiol Res. 2015;5(5):143-148.
Kibret M, Abera B. Prevalence and antibiogram of bacterial isolates from urinary tract infections at Dessie Health Research Laboratory, Ethiopia. Asian Pac J Trop Biomed. 2014;4(2):164-168.
Abejew AA, Denboba AA, Mekonnen AG. Prevalence and antibiotic resistance pattern of urinary tract bacterial infections in Dessie area, North-East Ethiopia. BMC Res Notes. 2014;7:1-7.
Das A, Banerjee T. Prevalence of urinary tract infections and susceptibility pattern of uropathogens in women of reproductive age group from North India. J Adv Med. 2015;4(1-2):5-9.
Sajed AN, Batool U, Iram S, Yousaf NW, Asghar MN, Khan S, et al. Prevalence of urinary tract infections and their antibiotic sensitivity in tertiary care hospital Lahore. IOSR J Dent Med Sci. 2014;13(12):57-61.
Al Mohajer M, Darouiche RO. Staphylococcus aureus bacteriuria: source, clinical relevance, and management. Curr Infect Dis Rep. 2012;14:601-606.
Baldwin CM, Lyseng-Williamson KA, Keam SJ. Meropenem: a review of its use in the treatment of serious bacterial infections. Drugs. 2008;68:803-838.
Dash M, Padhi S, Mohanty I, Panda P, Parida B. Antimicrobial resistance in pathogens causing urinary tract infections in a rural community of Odisha, India. J Family Community Med. 2013;20(1):20-26.
Lames H Almanseekanaa. Molecular Study of Enteropathogenic Escherichia Coli Isolation from Clinical Samples. Aca. Intl. J. Med. Sci. 2022: 1(1):06-14: https://doi.org/10.59675/M2022-02
Downloads
Published
Issue
Section
License
Copyright (c) 2025 Academic International Journal of Medical Sciences

This work is licensed under a Creative Commons Attribution 4.0 International License.